Can a Vasectomy Be Reversed?
Yes, a vasectomy can often be reversed—but success depends on several key factors, including how long it’s been since the original procedure, the surgical technique used during the vasectomy, and the skill of the surgeon performing the reversal.
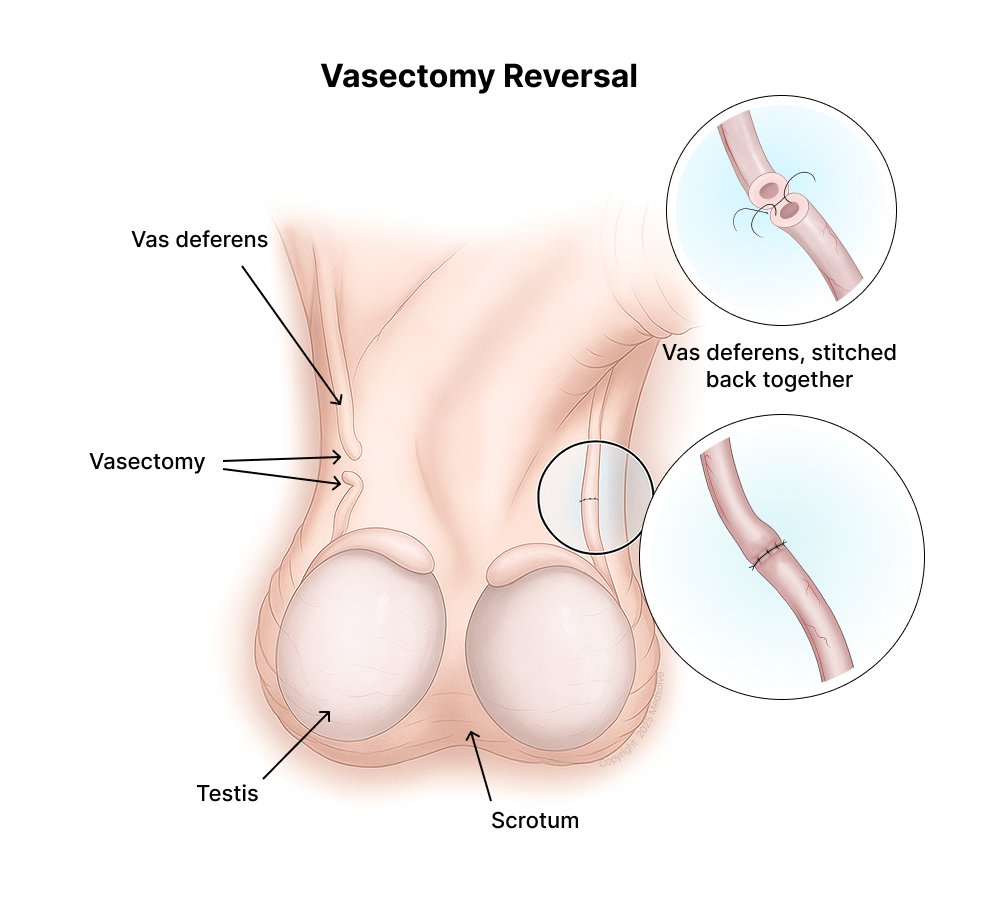
Understanding Vasectomy Reversal
A vasectomy reversal is a microsurgical procedure that reconnects the vas deferens—the tubes that carry sperm from the testicles to the urethra. Once reconnected, sperm can once again be present in the semen, which may restore fertility.
There are two main types of reversal procedures:
- Vasovasostomy: Reconnects the two ends of the vas deferens.
- Vasoepididymostomy: Connects the vas deferens directly to the epididymis when a blockage is found.
The type of procedure used depends on the individual’s anatomy and whether sperm are present in the vasal fluid at the time of surgery.
How Successful Is It?
Success rates vary, but here’s what the data shows:
- 75–97% pregnancy success rate if the reversal is done within 3 years of the vasectomy.
- 30–60% success if more than 10 years have passed.
Better outcomes are typically achieved when the original vasectomy was performed using a reversal-friendly technique—and when the reversal is done by a skilled microsurgeon.
My Technique: Designed for Reversibility
At our clinic, I use the no-scalpel, open-ended vasectomy technique with fascial interposition.
This method not only reduces recovery time and post-op discomfort, but also increases the likelihood of successful reversal later. The open-ended approach avoids pressure buildup, and fascial interposition lowers the risk of spontaneous reconnection—without compromising the potential for a successful reversal.
Final Thoughts
While vasectomy is intended to be a permanent form of contraception, reversal is possible—and in many cases, effective. If you’re planning a vasectomy, we’re here to help you understand your options and make the decision that’s right for you.